"Buy zitrotek with amex, infection smell".
By: M. Roland, M.B. B.A.O., M.B.B.Ch., Ph.D.
Deputy Director, Dell Medical School at The University of Texas at Austin
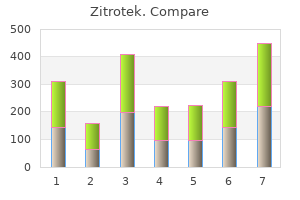
Moreover virus map zitrotek 100mg discount, the solution should be avoided by limiting the number of grafts rapid rotation damages the closer follicles antibiotics for uti uk order zitrotek with a visa, resulting in to 1 antibiotic resistance and farm animals order zitrotek 500 mg on line,200–1,400. The manual method is there- grafts can be performed in two sessions, leaving 1 day of rest fore more precise, even if a micromotor takes less time to between the sessions [22–24 ]. The promise of an • For limited areas of alopecia secondary to dermatologic almost scarless operation is alluring both for the patient and conditions the surgeon, even if this is not the case because in reality • In the treatment of wide cicatricial areas secondary to tra- there will be 1,000–2,000 diffuse, dot-like miniscars instead ditional harvest of the strip of a linear one. I consent to undergo medical and physical therapies that will answer depends on the size of the bald area, elasticity and be prescribed in the postoperative period, being informed hair thickness of the donor areas, and evaluation of future that otherwise I may compromise the procedure itself. I am aware that the quantity and quality of my hair is a ised or guaranteed good results: the final result cannot be primary factor for the final outcome of the procedure. After surgery I will According to the privacy law, I consent to be taken pre-, have permanent and visible scars, whose extent is not pre- intra- and postoperative pictures, which will have popular- dictable in advance (formation of visible, painful scars, scientific purposes. The procedure, as all other surgical procedures, is subject because of possible abnormal responses of my body. I considered appropriate and received comprehensive explana- Possible complications: All common complications of tions which I totally understood and that I have been satisfied of. Orentreich N (1959) Autograft in alopecias and other selected der- ing hair in the recipient site falls out. Ann N Y Acad Sci 83:463–479 is unpredictable, in the majority of cases the hair regrows 2. Ann Plast Surg 27(5):476–487 However, sometimes they do not all regrow, so it can 3. Marritt E (1984) Single hair transplantation of hairline refinement: a practical solution. J Dermatol Surg Oncol 10:962 be necessary to perform a second touch- up operation. Nordstrom R (1981) Micrografts for the improvement of the frontal –Microcysts: may occur in the recipient area at the base hairline after hair transplantation. Aesthet Plast Surg 5:97–101 of the implanted follicles, especially in people with 5. Transplant Forum Int 15:113–116 – Loss of sensibility: after surgery an alteration or tem- 7. Toscani M, Fioramonti P, Ciotti M, Scuderi N (2011) Single follicu- lar unit hair transplantation to restore eyebrows. Toscani M, Fioramonti P, Rusciani A, Scuderi N (2008) Hair trans- • Keloid formation plantation to restore pubic area. I give consent to the administration of anesthetics and I 771–784 am aware that there are risks to life and health as conse- 15. Dermatol Surg 23:785–799 micrografting as an approach to further refinement in hair trans- 17. Dermatol Surg follicular unit extraction hair transplantation with a powered punch- 28:720–728 ing device. Unger and Marco Toscani Scalp reduction can be defined as the surgical excision of A large series on scalp reduction was published by Bosley redundant scalp tissue from one or more areas of alopecia of et al. Since the 1930s, surgeons have used advancements published his first paper, making us aware that larger areas of and/or rotation flaps to reconstruct scalp defects after areas alopecia could be removed provided that extensive under- of malignancy or cicatricial alopecia have been excised. In mining, increased tension on closure, and galeotomies were patients with larger defects, serial excisions were success- incorporated. Significant contributions to this field have also fully used to remove areas that could not be excised in a been made by Norwood and Shiell [8], Nordstrom [9], single operation.
Electrical injuries to the intestine are not always diagnosed intraoperatively antibiotic kill curve protocol zitrotek 250mg overnight delivery, or their appearance leads the surgeon toward conservative treatment [43] antibiotic ceftin buy zitrotek 100 mg without prescription. It is suggested that burns less than 5 mm in diameter can be treated expectantly [44] fast acting antibiotics for acne order line zitrotek. If the area of blanching exceeds 5 mm, it is estimated that the thermal damage may exceed up to 5 cm from the apparent injury and resection should be considered [45]. Damaged bowel must be repaired or resected with or without a temporary colostomy as early as possible to minimize morbidity and mortality. Prevention of Bowel Injuries The most significant reduction in bowel complications during laparoscopic pelvic floor surgery will arise from preventing damage. The focus of attention should lie on careful adhesiolysis and enterolysis and the detection of injuries intraoperatively rather than postoperatively. A multidisciplinary group of Dutch surgeons recently performed a systematic review on the impact of adhesions in pelvic surgery. They reported on 2565 cases in 16 studies where adhesiolysis was required and reported an enterotomy rate of 5. The rate of enterotomy was also significantly lower if the surgery was performed laparoscopically (1. During adhesiolysis and enterolysis, sharp dissection with minimal diathermy will be beneficial in preventing inadvertent bowel damage. Careful inspections of the bowel for hematoma or serosal damage that may suggest breaches of the mucosa and the performance of the underwater test, if there is any concern regarding the integrity of the bowel, are all useful in allowing the intraoperative rather than postoperative diagnosis of bowel damage. The underwater test involves holding any area of the bowel suspected of damage under warmed saline looking for gas or bowel leakage. A rectal [49] and colon [50] injury were repaired laparoscopically without sequelae, and two small bowel injuries were diagnosed postoperatively and underwent subsequent laparotomy [51]. Bowel Preparation Bowel preparation prior to surgery was utilized—first, to remove the bulky intraluminal contents to improve surgical field vision and bowel handling, and second, to decrease the risk of peritoneal and wound contamination if the bowel was inadvertently opened. Bowel preparation 1516 results in the transfer of fluid and electrolytes to the bowel lumen that may result in hypokalemia and hypothermia and should be utilized perhaps only in those with higher risk of bowel injury such as those with known adhesions or diverticular disease. In comparison, 1 in 20 women in the colpopexy and urinary reduction efforts trial experienced significant gastrointestinal morbidity after open sacral colpopexy where closure of the peritoneum was optional. Of 322 women in the study, 19 had symptoms of possible ileus or small bowel obstruction; of these, 4 had reoperation for small bowel obstruction, 11 were readmitted for medical management, and 4 had a prolonged initial hospitalization for gastrointestinal symptoms [55]. In a recent publication comparing robotic and laparoscopic approach to sacral colpopexy, again where closure of peritoneum was optional, the rate of small bowel obstruction was 2. The question raised is whether the relatively simple task of closing the peritoneum after sacral colpopexy has a role in minimizing postoperative bowel complications and would be easily answered by a subanalysis of these two papers. Brosens reported that a gynecologist performing less than 100 laparoscopies a year had a five times higher rate of bowel injuries than those performing more than 100 laparoscopies a year [38]. Operating time declined rapidly after the first 30 cases and continued to decline before plateauing after 90 cases. Skills can be improved in a variety of means including training programs, skills workshops, and operating with colleagues. A gas filled urinary bag or blood in the urine means bladder trauma till proven otherwise and warrants careful laparoscopic inspection of the bladder distended to 300 mL and cystoscopy. Cystotomies should be repaired in two layers so that the bladder is watertight at 300 mL. After repair, cystoscopy should be performed with the laparoscope in place, to ensure that there are no other unrecognized injuries and that the ureters are patent.
500mg zitrotek sale. How to choose a replacement toilet seat.
In this manner antibiotic to treat mrsa 250 mg zitrotek visa, the morphology of the depending on the planned cartilage resection and on the nose is transformed with redistribution of the covering tis- possible dissection of the rear extension of the alar carti- sues that saddle the new structure by exploiting the healing lage virus gear order zitrotek 100 mg fast delivery. With curved blunt scissors ing it extramucosally from the osteocartilaginous skeleton the separation of the membranous septum and the region (extramucosal technique) [18 infection z cast order cheap zitrotek online, 20, 21 ]. The incision is then extended The intranasal access has the advantage of avoiding the toward the nasal spine on the basis of required exposure transcolumellar scar that sometimes may remain evident and the desired effect. A major release of the membranous and depressed, which may create marked psychological problems for the patient and also appears as a “stigma” of rhinoplasty [1, 11 , 16]. The endonasal technique avoids edema of the soft parts, which can persist over time; the risk of skin necrosis is also nonexistent. Any complications arising from inaccurate or unfortunate use of the open access can be much more serious and difficult to hide than those arising from the endonasal access. The advantages of open access are the excellent exposure of the anatomical structures, especially of the lower third of the nose, and the possibility to make their correction easier, especially in situations most difficult to resolve (eg, post-traumatic seri- ous nasal deformities or malformation, secondary and ter- tiary rhinoplasty). There is no precise rule about the time course of a rhino- plasty; each surgeon prefers and can choose a different suc- cession of surgical times. We prefer to treat primarily the middle third and the top, while other surgeons give prece- dence to the lower third of the nose (tip), treating the nasal dorsum later. We recommend performing muscle insertions determine the tip regression and the this type of approach in cases of thick skin, narrow nostrils, lowering of the upper lip; this action is taken in the event of and hard alar cartilage (Fig. The transcartilaginous incision allows resection of a part The transcartilaginous incision [3, 4, 10, 18] affects the of the alar cartilage, which is dissected with direct access up intermediate and lateral crura of the alar cartilage, allowing a to the triangular cartilage and the sesamoid cartilages. Next, elevation of the nasal skin mantle from the deep support structures is performed with a straight-blade scalpel for the pyramid sides and with a curved-blade scalpel for the dorsum. Alternatively, one may use blunt and curved scissors (Ragnell’s scissors) for the same dissection (Fig. The detachment involves a plane external to the perichondrium of the triangular cartilage and external to the periosteum of the frontal apophysis [10]. The cartilaginous resection is performed after the incision (b) Basic Rhinoplasty 605 Fig. Described by Eitnerin in 1932 in Austria and revised later by Fomon in 1939, Anderson in 1958, and gradually by other authors [9, 12, 18, 24 – 26], this technique separates the mucosa from the deep part of the triangular cartilage, the septum, and the nasal bones, passing in the subperiosteal and subperichondrial plane: In this way the osteocartilaginous structure is completely Fig. Furthermore, the lar cartilage extramucosal approach respects the mucosa, passing through a bloodless plane and allowing complete isolation (cavity closed) of any cartilage or bone grafts from the nose cavity. A second dissection involves the caudal margin: the lower intra- and postoperative bleeding, and decreased this will facilitate quadrangular resection when, toward the edema. Figure 16 highlights the resection lines for the osteo- end of the intervention, the desired rotation angle of the tip is cartilaginous dorsum with the extramucosal technique, evaluated [12, 16, 23, 24 ]. At this For the transmucosal technique the mucosa and the point, pushing downward toward the nasal cavities, the osteocartilaginous structure must first be sectioned, without 606 C. The Aufricht elevator is repositioned and, with the help of angled quadrangular scissors (about 130°), a quad- rangular strip of length and height corresponding to the pre- viously elaborate graphic project is resected (Fig. Meanwhile the triangular cartilages are remodeled and low- ered to the same height as the square. Resection of the osteocartilaginous structure must be carefully considered, and the resections must be parsimonious so as to avoid unsightly surgical outcomes.
The presence of any internal metal fragments antibiotic kill curve buy cheap zitrotek 500mg line, body-worn metal (jewelry) antibiotic for ear infection order zitrotek 500 mg overnight delivery, or stray metal objects in reach of the magnetic field also have to be excluded for the safety of the patient and the scanner antibiotics gas buy cheap zitrotek 500 mg on line. The patient undergoing scanning is placed in a confined environment, and this is problematic for patients prone to claustrophobia. Careful support for such patients and use of suitable medications according to hospital practice may be warranted. Gadolinium side effects may include headache, nausea, and temporary dizziness in 1%–5%. Gadolinium contrast medium should be avoided in patients with kidney disease (chronic or acute). Case reports of nephrogenic systemic fibrosis, leading to skin contractures and organ failure, have been described with gadolinium contrast in a minority of patients with preexisting severe renal dysfunction. For women in the first trimester of pregnancy, safety is uncertain, but it may be preferable to alternative options [6,7]. However, it is likely that there is degree of overlap between symptomatic women and asymptomatic nulliparous women [11]. The urethropelvic ligaments were reported to attach to the lateral aspect of the urethra to the medial aspect of the levator sling [12]. For some symptomatic women, bony changes may be evident: the transverse inlet can be wider, the intertuberous and interspinous diameters can be increased, the sacral length can be increased with a deeper curve, and the anteroposterior outlet can be narrowed [13]. The technology for 3-D imaging continues to develop, and progress in understanding clinical anatomy of the levator ani and bladder neck [4] will continue. The latter study reported the levator–symphysis gap as a marker for disruption of the attachment of the anterior puborectalis attachment. In primiparous women, around 20% have some degree of structural defect or deviation (Figure 38. Taken together, these findings would suggest that vaginal childbirth may weaken the urethral closure mechanism, thereby disposing the patient to urinary incontinence. Nulliparous African-Americans have significantly thicker levator ani muscles [18] and a higher urethral volume [19]. It has the advantage of detailed anatomical views of all three compartments at rest and during Valsalva. It is a straight line between the inferior border of the pubic symphysis and the last coccygeal joint. With these landmarks, it is possible to standardize and to grade the prolapse severity. It is widely recognized that the angle of pelvic inclination can change during specific maneuvers such as the Valsalva and Kegel maneuvers. This angle can also be affected by the way that an individual lies in the scanner (e. The optimal pelvic reference system should allow the investigator to compensate for these variations. TheH- line, from the inferior border of the symphysis to the posterior wall of the rectum at the level of the anorectal junction. The green circle denotes the urethral axis, which is vertical during straining and defection. The vagina is filled with sonographic gel (arrowheads); intra-anal full-thickness rectal invagination 576 (white arrow) at the level of the anal canal, thus impeding stool passage.