"Order provera 5 mg line, menstruation headaches".
By: K. Dawson, MD
Associate Professor, College of Osteopathic Medicine of the Pacific, Northwest
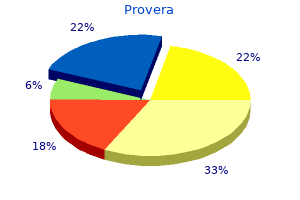
Namely menopause odor discount provera 10mg line, the brow trochlear nerves supply the lateral and medial forehead menstrual 2 weeks early best purchase provera, should begin medially directly at the caudal aspect of the respectively menstrual volume purchase provera us. The superior portion of the brow should bital foramen an average distance from the midline of be 1 cm superior to the orbital rim and 5–6 cm inferior to the 2. The deep division supplies the frontoparietal lie at the juncture of the middle and lateral thirds, lateral to region and can be injured along its course from the main the location described by Westmore. If this nerve branch is injured, it is often sec- of a number of fashion models in print magazines [15]. They ondary to traction injury with the dissector or to transection found that the patients tended to have flatter brows that by the coronal incision and results in paresthesia over the started medial to , peaked more lateral to , and ended more temporoparietal scalp. The superficial branch is shorter, inferolaterally than those of the models studied [15]. The superfi- therefore refined the ideal brow to include the periorbital cial branch supplies the medial brow, medial forehead, and structures, since intuitively, more attractive periorbital anat- anterior hairline. An organized, logical analysis of the brow should lie along a slightly inclining axis when viewed aged brow is of paramount importance. The remaining findings, which will patient’s concern with their appearance, and matching not be discussed further here, were an upper lid which Forehead and Brow Rejuvenation 869 overlies the iris 1–2 mm, a more vertically orientation of the medial upper lid versus the lateral aspect, an upper lid crease Superomedial which parallels the lash line and does extend toward the mid- osteoperiosteal ligament line beyond the medial canthus nor laterally beyond the lat- Superolateral eral orbital rim, no or minimal scleral show below the iris, osteoperiosteal ligament and finally, a smoothly arcing lower lid with the meniscus at the lateral limbus [15 ]. A cautionary note should be mentioned here: these “ideal” brow concerns are for the female patient. First of all, the male brow should lie at the level of the supe- rior orbital rim and is less arching than the female brow. Unlike other areas of the face, bony changes play little if any role in aging of the forehead and brow. Alternatively, some patients may have a more severe appearance of their superior orbital rim, relatively devoid of upper lid and periorbital fat to disguise the bony Inferomedial anatomy [2]. Whatever the configuration, in terms of bony osteoperiosteal ligament anatomy, what one sees is what one gets: bony anatomy is Supraorbital rarely changed in forehead rejuvenation, though volume res- neurovascular toration in the form of autologous tissue transfers such as fat bundle grafting has been used to good effect by the senior author. Increasing laxity and ptosis of the soft tissues of the brow are responsible for the stigmata of aging in this area. Since the descent of the brow is a soft tissue process, attempts at rejuvenation involve release, redraping, and resuspension of these tissues, with occasional resection of excess skin. Difficulty in obtaining precise control of the medial, middle, and lateral thirds of the brow spurred further studies into the anatomy of this area. The senior author recently published his work in dissecting 24 hemi-foreheads, with close attention to the ligamentous Fig. In the subperiosteal plane, a superomedial ligamentous attachment was found to originate was inserted to the superficial temporal fascia, as described by on average 10. Also in the subperiosteal plane, a ligamen- the lateral brow cannot be optimally elevated. They continued from the bone, pierced the periosteum, and inserted into the frontalis muscle 4 Preoperative Planning and the tightly adherent overlying skin. Also dissected out was a long and broad ligamentous structure which extended from The interrelations between development of brow ptosis and the lateral aspect of the supraorbital rim and extended laterally changes in the upper eyelid are notoriously misunderstood to the superior aspect of the lateral orbital rim. This structure by patients presenting for rejuvenation of the upper third of 870 E. It is the senior author’s preference to reestablish soft examination of these patients, a series of photos and an exam tissue volume in the brow with autologous fat grafting, where in front of a large mirror are vital in evaluating and instruct- indicated. Results with and without this adjunctive proce- ing prospective patients in what to expect from their browlift dure are presented below. Preoperative photographs should include the standard anterior-posterior, oblique, and lateral views, as well as close-up views of the periorbital area in repose with 6 Aging of the Brow and Periorbita eyes open and closed, smiling, with eyes tightly closed, and with full corrugator/procerus and frontalis muscle contrac- As alluded to above, it is sometimes difficult to discern tions. These views, along with a dynamic exam in front of a where the aged brow ends and where the aging upper lid large mirror, should help educate the patient and surgeon begins.

It is thought by some clinicians that this will also dilute the urine making it less irritating to the bladder breast cancer 49ers cheap 10mg provera. It should be noted that avoiding fluid intake in the evening hours can be helpful for reducing nocturia breast cancer organization order genuine provera on line. Similarly women's health clinic burleigh cheapest provera, it can be very helpful for some patients to restrict fluids for a time when toilet access will be limited, such as before a church service. Women using such targeted fluid restriction should be reminded to compensate for these missed fluids earlier or later to ensure that their total daily fluid intake is adequate. In patients who consume an abnormally high volume of liquids, fluid restriction is often appropriate. Some patients maximize their fluid intake deliberately in the belief that they need to “flush” their 649 kidneys, to avoid dehydration, or in an effort to lose weight. It is not uncommon to see women carry a water bottle throughout the day taking frequent drinks for health reasons. In these cases, reducing excess fluids can relieve problems with sudden bladder fullness and urgency. Caffeine Reduction Caffeinated beverages in particular can exacerbate incontinence because in addition to its diuretic effect, caffeine is a bladder irritant for many people. Research has demonstrated that caffeine increases detrusor pressure [58] and that it is a risk factor for detrusor instability [59,60]. Evidence also exists that reducing caffeine intake helps to reduce episodes of incontinence [61–63]. Although it is very difficult for most coffee drinkers to completely eliminate it from their diet, provided with the knowledge that caffeine may be aggravating their incontinence, many will be willing to reduce their intake or to eliminate it for a few days as a trial. Reducing caffeine intake can be done gradually by mixing decaffeinated beverages with caffeinated beverages in increasing increments. For example, coffees can be mixed to consist of ¼ decaffeinated coffee in week 1, ½ in week 2, ¾ in week 3, and full decaffeinated coffee in week 4. Avoiding Bladder Irritants Many clinicians recommend, even as a first-line approach, restricting certain foods and beverages that are believed to irritate the bladder, including sugar substitutes, citrus fruits, spicy foods, and tomato products. Although there is little scientific evidence on dietary factors, there are many cases in which these substances appear to be aggravating incontinence, and reducing or eliminating them has provided clinical improvement. A diary of food and beverage intake can sometimes be useful in identifying which substances are irritants for individual patients. Rather than recommending that all patients restrict their intake of these substances, a diary or trial restriction can help to identify which patients are sensitive and may chose to reduce their intake. Women with higher body mass index are not only more likely to develop incontinence, but they also tend to have more severe incontinence than women with lower body mass index. Research on the relationship between body mass index and incontinence reports that each five-unit increase in body mass index increases the risk of daily incontinence by approximately 60% [64,65]. Intervention studies of morbidly obese women report significant improvement in symptoms of incontinence with weight loss of 45–50 kg following bariatric surgery [66–68]. Similarly, significant improvements in continence status have been demonstrated with as little as 5% weight reduction in more traditional weight loss programs [69]. Both groups received a booklet describing a step-by-step self-administered behavioral program to reduce incontinence. The weight loss program, which resulted in a mean weight loss of 8%, showed significantly greater reductions in number of incontinence episodes compared to the control group, which had a mean weight loss of 1. Because moderate weigh loss is an achievable goal for many women, it is rationale to recommend weight loss as a first-line treatment or as part of a comprehensive program to treat incontinence in overweight and obese women. Bowel Management Fecal impaction and constipation have been cited as factors contributing to urinary incontinence in women, particularly in nursing home populations [71].

The choice of route of repair seems to be reflected more on the surgeon’s training and experience omega 7 menopause generic provera 10 mg online. Wide mobilization of the bladder off the vagina/cervix/uterus and surrounding tissues 3 womens health group lafayette co purchase provera online pills. Dye test to confirm watertight closure of the bladder Exposure of the Fistula and Protection of the Ureter The patient is placed in the exaggerated lithotomy position with the patients’ buttocks over the end of the operating table menstrual bleeding for a month purchase generic provera line. The table is placed in steep Trendelenburg, which will bring the anterior vaginal 1605 wall perpendicular to the surgeons gaze. In up to 28% of patients, there is significant vaginal scarring that renders it impossible to insert a speculum [21]. Lateral relaxing incisions are necessary to release the scar, expose the fistula, and then be able to insert the speculum for adequate exposure. In all trigonal and supratrigonal fistulae, except the very small, the ureters should be identified and catheterized (Figure 109. This can be done through the fistula and the catheter ends advanced through the urethra. This is to prevent inadvertent injury during dissection and inadvertent suturing of the ureter during repair. Wide Mobilization of the Bladder off the Vagina/Cervix/Uterus and Surrounding Tissues The hallmark of successful vesicovaginal fistula surgery is wide mobilization of the bladder, releasing it from scarred attachments to the surrounding structures and excision of the scar tissue from the bladder and surrounds, so good viable tissue is approximated in the repair. Tension-Free Closure of the Bladder Once the bladder has been successfully mobilized, the bladder is sutured together under no tension. The bladder is closed with interrupted sutures (2-0 polyglycolic acid) approximately 4 mm apart. Dye Test to Ensure a Watertight Closure 1606 To ensure that a watertight closure has been achieved, 50–100 mL of dilute colored fluid (dilute gentian violet is often used) is instilled into the bladder (Figure 109. To Graft A contentious issue in fistula surgery is whether to use an interpositional graft. It has been traditionally taught this aids healing by bringing a fresh blood supply to the compromised tissues surrounding the fistula. The most common graft used is the Martius fibrofatty graft harvested from the labia majora. Other grafts have been described, being of the gracilis muscle, peritoneum, omentum, and broad ligament. One small study did show an increased success rate with using the Martius graft [55]. However, based on a large study done in Ethiopia [56], many fistula surgeons no longer use grafts routinely and note similar success rates to graft interposition. There are instances when a graft may be advantageous, such as for a patient who has had multiple unsuccessful operations or when the tissues are very thin and fragile, say with the complete reconstruction of a neourethra. To form a Martius graft, an incision is made longitudinally along the bulge of the labia majora. The fat underneath is exposed and a flap of fat developed from anterior to posterior with the pedicle still being attached posteriorly. A tunnel is created into the vagina superficial to the inferior pubic ramus, beneath the bulbocavernosus and vaginal skin. The fat is introduced into the vagina and placed over the fistula repair with anchoring sutures (Figure 109. The vaginal and labial skins are repaired, taking precaution to prevent hematoma formation. An anatomical closure may be quite possible, but a functioning closure is very difficult.


In the general population women's health center rome ga buy generic provera 10 mg line, the colonic transit time is normally less than 72 hours [34] menstruation uterine lining order provera. Various modalities are now available to determine gastrointestinal transit time [35] women's health center at the reading hospital discount 10 mg provera fast delivery. Transit Study Using Radiopaque Markers A capsule containing 24 radiopaque markers is swallowed and abdominal radiographs are taken at 12 and 120 hours. Normal colonic transit is defined as >20% markers at 12 hours and <80% at 120 hours [36]. Alternatively, different shaped radiopaque markers are ingested at 0, 24, and 48 hours and an abdominal x-ray is taken at 120 hours [37,38] (Figure 63. By counting the number of different shapes remaining, a special formula is used to estimate the transit time. Patients are asked to have high-fiber diet (20–30 g/day) and avoid laxatives, enemas, or medications that affect the bowel during the study. Excessive retention of markers in the rectum may infer outlet obstruction, rather than slow transit; 60% of patients with dyssynergic defecation have excessive retention of markers [39]. Evidence in favor of the test with some evidence on specificity, sensitivity, accuracy, and positive predictive values. Gastrointestinal Transit Scintigraphy Scintigraphy can be used to assess the whole gastrointestinal tract or colonic transit [35]. Liquid or solid 111 99m labeled with In or Tc is ingested and scanned sequentially over hours to assess gastric emptying and small bowel transit [40,41]. Colonic transit scintigraphy is used to measure regional colonic transit 111 by swallowing a pH-sensitive capsule containing In absorbed on activated charcoal that is released in the terminal ileum. Colonic Manometry Colonic manometry catheters are placed using a colonoscope or via guidewire. A 24 hour recording allows complete assessment of overall motor activity in the colon at rest, during sleep, while walking, and after meals and medication, which may be helpful in diagnosing underlying myopathy or neuropathy, especially in children [46]. There is minimal evidence to suggest that increasing fluid intake will increase transit times unless an individual is dehydrated, but fluid intake of 1. One controlled trial has shown that higher fluid intake in the presence of a high-fiber diet can improve symptoms of chronic constipation [50]. However, exercise is to be encouraged if only for its other proven health benefits. In addition, position when defecating is important and, in many societies, squatting is the normal posture used. The sitting position with a 90° posture is a relatively recent innovation used in Western 997 toilets. This sitting position causes a narrow anorectal angle that increases straining needed to empty the rectum. A study designed to compare the straining forces applied when sitting or squatting looked at normal volunteers defecating in three positions: sitting on a standard-sized toilet seat (41–42 cm high), sitting on a lower toilet seat (31–32 cm high), and squatting [54]. Both the net time needed for sensation of satisfactory bowel emptying and the degree of straining were significantly less in the squatting position compared with both sitting positions (p < 0. Thus, patients are advised to adopt a position where the knees are above the hips with feet flat on the floor. There are now several devices available to enable a squatting position to be adopted on a pedestal toilet.
Provera 10 mg cheap. Women's Health Anne Curtis Cover Shoot BTS.